8 Lived Experiences of Racism in Medicine and Research
Maternal Mortality Rates
In the United States, maternal mortality rates are significantly higher for Black women compared to White women, regardless of income or educational status. A report revealed that Black women experience severe maternal complications at three times the rate of White women, and this disparity persists even after accounting for factors such as education, poverty, and obesity. The study also found similarly high rates among Hispanic women compared to White women.[1]
Maternal mortality rates, by race and Hispanic origin: United States, 2018–2021
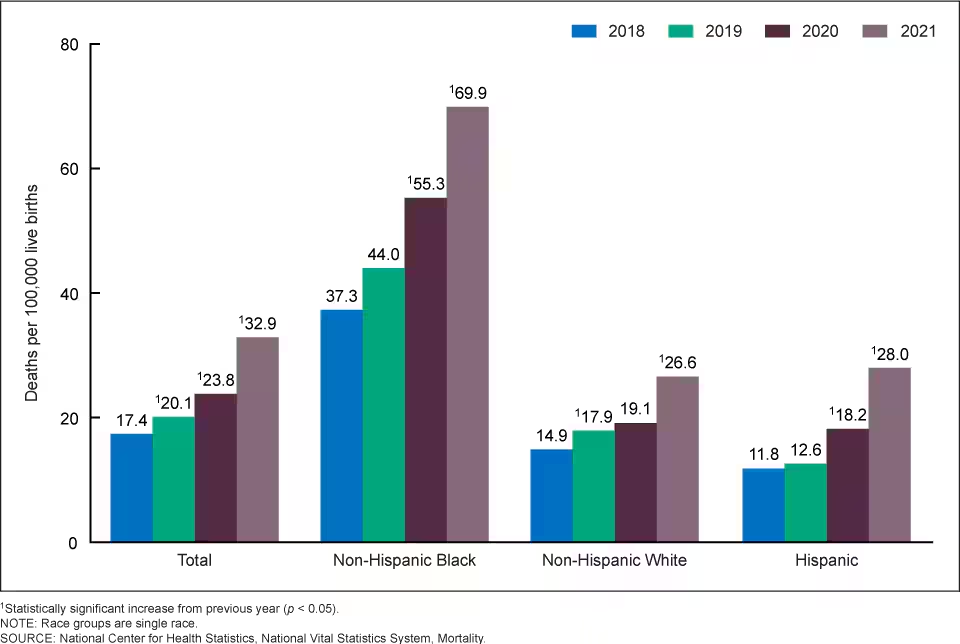
“According to the CDC, black mothers in the U.S. die at three to four times the rate of white mothers, one of the widest of all racial disparities in women’s health. “Put another way,” the report explained, “a black woman is 22% more likely to die from heart disease than a white woman, 71% more likely to perish from cervical cancer, but 243% more likely to die from pregnancy- or childbirth-related causes[2].”
The common thread in Black maternal mortality includes:[3]
- Silencing Black women’s pleas for medical help
- Unconscious bias against Black postpartum women
- Dismissing the health care needs of pregnant and postpartum Black women
- Not believing that Black women know their bodies well enough to know when something is wrong
Shalon Irving’s Story
Shalon Irving 1980 – 2017
“I see inequity wherever it exists. I am not afraid to call it by name and work hard to eliminate it. I vow to create a better earth.” — Shalon Irving

The article “Black Mothers Keep Dying After Giving Birth. Shalon Irving’s Story Explains Why” provides details and commentary on the death of Shalon Irving, PhD, MPH, MS, CHES. As an epidemiologist at the Centers for Disease Control and Lieutenant Commander in the US Public Health Service Commissioned Corps, Dr. Irving was an advocate for health equity who held a B.A. in sociology, two master’s degrees, a dual-subject Ph.D., stellar health insurance, and a vast and supportive network of family and friends. Yet, despite all of these privileges and advantages, she was not able to overcome the racial and health disparities that caused her to fall victim to the alarming statistic of the increased rate of black maternal death in the United States. Three weeks after giving birth to her daughter, Dr. Irving was dead.
Although she visited the doctor three times during the last week of her life for the same symptoms, and each time her blood pressure was recorded as elevated, she was repeatedly ignored and sent home. On January 24, 2017, Dr. Irving suffered a sudden cardiac arrest at home, just twenty-one days after giving birth to her daughter and only six hours after returning from yet another visit to her medical providers, during which she had pleaded for help. An autopsy revealed that her cause of death was heart damage caused by hypertension, a treatable condition.
Read the article and listen to the story on NPR below.
Hear Dr. Irving’s Story from her mother Wanda
“During the last week of her life, Shalon went to the doctor 3 times for the same symptoms…I lost my vibrant, beautiful, intelligent best friend and daughter because she wasn’t heard.” — Wanda Irving, mother of Shalon Irving
Additional Reading on Shalon Irving’s life, legacy, and tragic death
- Purnell, T. S., Irving, W., Irving, S., Underwood, L., McDonald-Mosley, R., Ibe, C., … & Bowie, J. (2022). Honoring Dr. Shalon Irving, a champion for health equity. Health Affairs, 41(2), 304-308. — https://www.healthaffairs.org/doi/10.1377/hlthaff.2021.01447
- A National Disgrace: Black Maternal Death
- The Death of a Young Black Mother Brings Attention to the Issue of Racial Health Disparities
Kira Dixon Johnson’s Story
“We walked in on what was expected to be the happiest day of our lives, and we walked straight into a nightmare.”
Hear Kira’s story, as told by her husband, Charles.
“Sunshine personified,” is how Charles Johnson IV describes his wife, Kira.
“We’re talking about a woman that raced cars, that ran marathons. She spoke five languages fluently. She was a skydiver. She had her pilot’s license. Everything she put her mind to, she did. She had this incredible infectious energy. She walked into a room and she would light it up. Yea, she’s just my earth angel. We just really were in such an amazingly happy place. We had grand plans of just raising kids that would change the world.” As Charles reflects on being first-time parents to their son Charles Johnson V, he explains, “We enjoyed it. It was a really, really cool time for us.”
In April of 2016, Kira was in perfect health and had experienced a textbook pregnancy as she prepared to deliver their second child. Doctors recommended a cesarean section since that is what she had the first time around. Shortly after Kira and Charles’ son Langston was born, Kira began experiencing complications. Charles noticed that the fluid in her catheter was turning pink, indicating the presence of blood. This was around 4pm and doctors stated that they would perform a CT scan. By 7pm, Kira was shivering uncontrollably, and ultrasounds showed that her abdomen was filling with fluid. Her CT scan had not been done yet. Increasingly concerned about his wife, Charles approached a nurse about Kira’s condition to ask for help and recalls being told, “Sir, your wife just isn’t a priority right now.” It was not until midnight that doctors took Kira in for surgery. The last thing Kira said to Charles was, “Baby I’m scared.” Having known Kira to be fearless, this was not a sentiment she had ever expressed or showed to him before.”[6]
Excerpted text from When Alarm Bells are Silenced: Black Maternal Mortality and Kira Johnson’s Story
Krystal Anderson (1983 – 2024)

Krystal Anderson, a former Kansas City Chiefs cheerleader and software engineer, was awarded a patent for developing software that assesses the risk of postpartum hemorrhage. Throughout her career, she contributed significantly to improving healthcare and advocated for Black women in STEM and in women’s health.
Krystal and her husband tragically experienced the stillbirth of their first child in 2022. Approaching her next pregnancy with great caution, she had uterine fibroids removed to reduce the risk of another loss. At sixteen weeks into her second pregnancy, she underwent a cerclage procedure to support the viability of her cervix. At her 20-week checkup, she was placed on semi-bedrest in hopes of reaching 22 weeks. Later in her 20th week, Krystal returned to the hospital with back pain, and during testing to determine the cause, doctors found no fetal heartbeat. Her baby was no longer viable.
Hours after receiving the devastating news, Krystal developed a fever and began showing signs of severe sepsis. She underwent surgery to deliver her stillborn daughter, but afterward required a ventilator and dialysis due to kidney, liver, and lung failure. Several days later, Krystal succumbed to complications related to sepsis.
References and more readings
https://www.yahoo.com/news/longtime-kansas-ity-chiefs-cheerleader-053322425.html
https://www.chiefs.com/news/the-life-legacy-and-sparkle-of-krystal-anderson
As part of a video series by the Brookings Institution highlighting race-based disparities or discrimination in public policy, Christen Linke Young asks readers to:
“Try to imagine what would happen if white mothers and white babies were dying at the rate of Black mothers and Black babies.”
Read the article here: There are clear, race-based inequalities in health insurance and health outcomes
Giving life should not be a death sentence for black women. — Dr. Shalon’s Maternal Action Project
The human toll of racism is profound, tearing apart individuals, families and communities and creating deep and lasting harm that reverberates through generations.
Sickle Cell Disease
Sickle cell disease is an extremely painful, debilitating, and potentially deadly condition that affects mainly African Americans. The genetic mutation that causes sickle cell disease originated on the African continent as a protective adaptation against malaria. As a result of the transatlantic slave trade, nearly all sickle cell disease patients in the United States are Black.
In a perspective published by the New England Journal of Medicine, authors Power-Hays and McGann state that:
“There may be no population of patients whose health care and outcomes are more affected by racism than those with sickle cell disease (SCD). Patients with SCD are too often marginalized and dismissed while seeking medical care when their bodies hurt, and they cannot breathe.”
Quoted text from When Actions Speak Louder Than Words — Racism and Sickle Cell Disease
Sickle Cell Anemia: A Patient’s Journey
The implications of sickle cell disease within a racialized society are vast and particularly harmful. For example, although sickle cell disease affects three times as many individuals as cystic fibrosis, a condition that primarily affects White Americans, research on cystic fibrosis has received seven to ten times more funding per patient. This disparity has slowed the development of treatments, as evidenced by the Food and Drug Administration’s approval of only four medications for sickle cell disease compared to fifteen for cystic fibrosis.
Pain crises, which result from blockages in blood flow, are the most common manifestation of sickle cell disease. The pain often requires hospitalization and the prompt administration of powerful opioid medications. However, because of the long-held belief that Black people are less sensitive to pain, combined with the persistent media portrayal of African Americans as drug users and related stereotypes, many individuals in the midst of a pain crisis are turned away with either no treatment or inadequate treatment. This can result in organ and tissue damage, decreased quality of life, and a higher risk of death from complications related to the crisis. Despite these risks, many patients choose to forgo care to avoid mistreatment by medical professionals.
References
- Sickle Cell Crisis https://www.ncbi.nlm.nih.gov/books/NBK526064/#article-29014.s8
- https://www.youtube.com/watch?v=2CsgXHdWqVs&t=4s
- Koltata, Gina. These Sisters with Sickle Cell Had Devastating, and Preventable, Strokes. New York Times. 23 May 202. https://www.nytimes.com/2021/05/23/health/sickle-cell-black-children.html
These Sisters With Sickle Cell Had Devastating, and Preventable, Strokes
“Kyra and Kami never got a simple test that could have protected them. Their story exemplifies the failure to care for people with the disease, most of whom are Black[7].”

“It was 4 a.m. on a Sunday when Dana Jones heard an ominous sound, barely audible over the whirring of box fans, like someone struggling to breathe. She ran down the hall and found her daughter Kyra, age 12, lying on her back, gasping for air. Terrified, she called 911.
A police officer, the first to arrive, dashed into Kyra’s bedroom, threw the slender girl over his shoulder and laid her on a leather sofa in the living room. He asked her mother, an oral surgery technician, to give her CPR.
Kyra’s lips were ice-cold. An ambulance whisked the girl to Methodist Children’s Hospital, where staff members swarmed her and put her into a medically induced coma.
Kyra, who has sickle cell, had suffered a devastating stroke — her second — a common complication of this inherited disease, which afflicts 100,000 Americans, most of them Black. She most likely would never have had the strokes if she had been given an annual screening test and treatment proven more than two decades earlier to prevent nine out of 10 strokes in children with the disease and recommended by the National Institutes of Health. But like countless other children with sickle cell, she was never screened.”
Excerpt from New York Times Article: These Sisters With Sickle Cell Had Devastating, and Preventable Strokes
To further underscore the disparities in treatment and care, the article states: “A third as many Americans have cystic fibrosis, a genetic disease of comparable seriousness to sickle cell but one that primarily affects White children, yet it receives seven to eleven times more research funding per patient. This results in disparate rates of medication development, according to a recent opinion piece in The New England Journal of Medicine. Only four medications are approved by federal regulators for sickle cell, and 15 for cystic fibrosis.”
Consistent with this finding, a study conducted by the Centers for Disease Control and Prevention reported that fewer than half of patients diagnosed with sickle cell disease are screened for stroke, a common complication that can shorten lifespan by more than 20 years.[8]
- Severe Maternal Morbidity ↵
- https://www.nysna.org/national-disgrace-black-maternal-death ↵
- https://smcdoulas.com/black-mothers-are-dying/ ↵
- https://www.cdc.gov/maternal-mortality/php/data-research/mmrc-2017-2019.html ↵
- https://www.nytimes.com/interactive/2023/02/12/upshot/child-maternal-mortality-rich-poor.html ↵
- https://www.instituteforchildsuccess.org/when-alarms-are-silenced-black-maternal-mortality-and-kira-johnsons-story/ ↵
- https://www.nytimes.com/2021/05/23/health/sickle-cell-black-children.html?unlocked_article_code=1.i08.zlhF.z30GaGtxvtwt&smid=url-share ↵
- https://www.usnews.com/news/health-news/articles/2022-09-20/study-too-few-kids-with-sickle-cell-get-stroke-screen-care ↵

